For healthcare professionals
Let’s curb the syphilis epidemic together.
Empower your community with reliable, accessible testing solutions.
Contact Us
How to use the First To Know® Syphilis Test
Watch instructional videoRead First To Know resources for more information
How First To Know
can help with public health testing
In the U.S., syphilis disproportionally affects certain minority populations, as well as the population of men who have sex with men (MSM). Testing is a critical tool in combating the syphilis epidemic. By increasing access to testing, we can address health disparities and work toward curbing the syphilis epidemic.
Be the first to know about your health
What is the First To Know Syphilis Test?
The First To Know Syphilis Test is a home-use fingerstick blood test for the detection of antibodies to the bacteria that cause syphilis. It yields an in-home result—in minutes.
See detailed instructions to perform the test.
1

Stick your finger with the provided lancet.
2
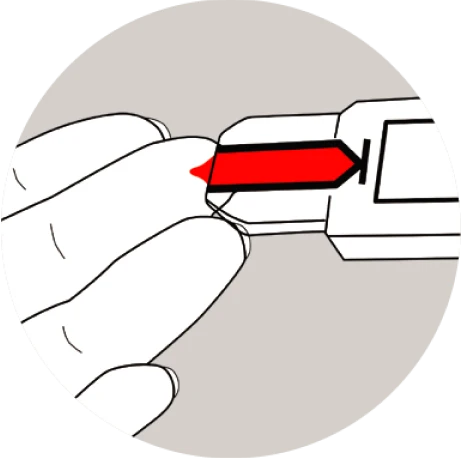
Touch the test cartridge to your finger to let a drop of blood enter the cartridge.
3
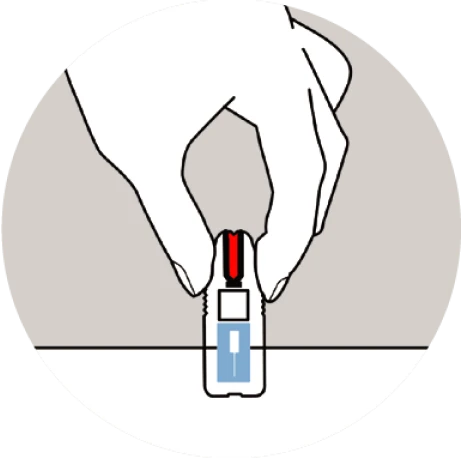
Tap the cartridge twice and lay it flat.
4
Wait 15 minutes for your in-home result.
Curb the syphilis epidemic with
First To Know
Learn More
As the only over-the-counter test for syphilis, the First To Know Syphilis Test is easy to use and can be taken anywhere, anytime. Local health clinics and public health programs can leverage the First To Know Syphilis Test to expand testing efforts through various initiatives such as:
Summary of First to Know Syphilis Test Clinical Study Results
93.4%
Positive Percent Agreement (PPA)
(95% confidence: 87.0% – 96.86%)
99.5%
Negative Percent Agreement (NPA)
(95% confidence: 98.9% – 99.8%)
Overview of the clinical study
- A multi-site study conducted from September 1, 2021, to October 17, 2023, at 6 geographically diverse clinical sites.
1,424 subjects from low-prevalence clinics participated. - Lay users performed the test using self-drawn fingerstick blood and were assessed for ease of use in a simulated home environment.
- Venous blood samples were tested by three FDA-cleared comparator tests.
- Comparator positive was established by 2 out of 3 positive results using these reference tests.
Total subjects in the final analysis: 1,270
Talk to your patients
about syphilis
With syphilis rates rising in the U.S., healthcare professionals play a critical role in curbing the spread of STIs by discussing sexual history and STI screening with their patients. According to the CDC, A sexual history should be taken as part of routine health care, as well as when there are symptoms or physical exam findings suggestive of STIs.*
Some patients may not be comfortable talking about their sexual history, sex partners, or sexual practices. It’s important to reassure them that taking a sexual history is a normal and essential aspect of comprehensive medical care. In some cases, simply offering all testing options, as opposed to specific STIs and diseases, may be the best approach.
Read the CDC guide to taking a patient’s sexual history for a complete guide on how to talk about sexual wellness with your patients.
Correlation with HIV
and syphilis
According to CDC, in 2022, approximately 36% of the MSM population with primary and secondary (P&S) syphilis also had HIV.** Members of the MSM population who are HIV-negative and diagnosed with P&S syphilis are more likely to get HIV in the future, as syphilis sores may make it easier for HIV to enter the body. Additionally, having HIV and another STI may also increase the risk of HIV transmission.***
If you have patients with HIV, read more information from the CDC about syphilis among persons with HIV.
*CDC Guide to Taking a Sexual History
** National Overview of STIs, 2022
*** HIV.gov Syphilis and People with HIV
Syphilis is surging
The need for syphilis testing
Rising rates
Syphilis rates in the U.S. have reached a level not seen since the 1950s—with cases increasing by nearly 80% between 2018 and 2022, according to the CDC. With rapidly rising rates of the disease, sexually active people could be at risk, especially because initial symptoms of syphilis can often be painless or go unnoticed.*
*U.S. Centers for Disease Control and Prevention
Learn MoreWho should be tested?
The CDC recommends the following populations be tested for syphilis:
Learn MoreAdditionally, The CDC recommends regular testing for people who are sexually active and: are taking pre-exposure prophylaxis (PrEP) for HIV prevention, have partner(s) who have tested positive for syphilis, and/or have certain risk factors for syphilis, like living in a community with high rates of syphilis.
If your patient tests positive using the First To Know Syphilis Test
Following a positive result from the First To Know Syphilis Test, healthcare professionals should conduct confirmatory testing by following the CDC guidelines for syphilis testing.
Results of testing with the First To Know Syphilis Test will likely be positive for individuals previously diagnosed with syphilis, even if they were successfully treated. The First To Know Syphilis Test cannot determine whether there has been a re-infection with syphilis.
See the CDC laboratory recommendations for syphilis testing.
See the traditional and reverse algorithms for syphilis screening from the CDC.

Find Out Now
Ordering the First To Know Syphilis Test
If you are a retailer, distributor, healthcare professional, or public health professional looking to place an order or learn more about our products, please contact us.
Contact Us
How It Works
The science behind the First To Know Syphilis Test
The First To Know Syphilis Test is a qualitative rapid membrane immunochromatographic assay for the detection of Treponema pallidum (syphilis) antibodies in human whole blood (capillary). To run the test, a fingerstick (capillary) blood sample is collected into the fill zone of the test cassette. The sample flows into a dry porous test strip composed of a plasma-separating membrane and a series of analytical membranes.
The sample first passes through the plasma-separating membrane, which binds the erythrocytes in whole blood sample to prevent them from interfering with the test. The membrane also contains two separate colloidal gold conjugate materials: syphilis recombinant protein conjugated with colloidal gold and Rabbit IgG conjugated with colloidal gold which are solubilized in the plasma as it continues to move into the device.
If positive, the syphilis specific antibody in the test sample binds to the recombinant syphilis antigen absorbed to gold in the upstream region of the test strip and the complex is captured by immobilized syphilis antigen striped at the test band location, as it flows downstream. The appearance of a visible test band indicates the sample contains a detectable level of syphilis antibody. Rabbit IgG conjugated with colloidal gold will flow past the test band region and bind to the polyclonal anti-rabbit antibody in the control band location of the analytical membranes, resulting in the appearance of a procedural control line.
